|
by Isabeau Doucet
 I
contracted cholera two years ago by the breezy beaches of Port
Salut, while attempting to escape burnout, a broken heart, and
the lingering pangs of Dengue fever in Port-au-Prince, Haiti’s
capital. I
contracted cholera two years ago by the breezy beaches of Port
Salut, while attempting to escape burnout, a broken heart, and
the lingering pangs of Dengue fever in Port-au-Prince, Haiti’s
capital.
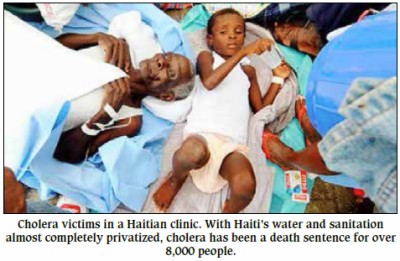
Cholera’s not a whole lot different from food poisoning and is
no big deal if you have a clean toilet, potable water, know how
to treat it, and aren’t malnourished.
But in
hunger-wracked Haiti, where there is no sewage system and where
water and sanitation are almost completely privatized, cholera
has been a death sentence for over 8,000 people. According to a
host of scientific studies (including the UN’s own
investigators), the South Asian strain of the disease was likely
imported by UN troops from Nepal in October 2010. Having
sickened over 640,000, it is now the worst cholera epidemic in
modern history.
A week before the
long-delayed release of an international $2.2 billion 10-year
eliminate-cholera plan at the end of February, the UN rejected
outright a legal claim filed by over 5,000 cholera victims
seeking financial compensation, an apology for the UN’s gross
negligence, and a commitment that the world body rebuild Haiti’s
water and sanitation infrastructure.
Invoking immunity
under its1946 convention, the UN snubbed the suit as “not
receivable.” It has not apologized and has committed only 1%
($23.5 million) to the plan, recommending Haiti get the rest
from the “private sector” or from “major venture philanthropist
individuals,” according to Nigel Fisher, the new head of the UN
military occupation force in Haiti known as MINUSTAH.
"Combating water
born diseases, cholera, is actually a good investment if you
want to attract investors," Fisher added.
With some 9,000
armed soldiers and police officers, MINUSTAH had an annual
budget of over $800 million last year. Its current one-year
mandate ends on Oct. 15, 2013.
In a country
where nearly 80% of people live on less that $2 a day, the
water-and-sanitation-access-for-profit model has left over 80%
without adequate sanitation and nearly a third without potable
water.
"When
you look at the price of a bag of water, supposedly treated, it
costs more to buy a gallon of water when you're poor than a
gallon of diesel fuel," said veteran political activist Patrick Elie, looking at water vendors weave through traffic and crowds
to sell as many 300ml 5 cent bags of iced water as possible
before they turned hot under Haiti’s blistering sun.
Those in tent
camps and shanties who can’t pay for a toilet, defecate into
plastic bags that end up in the nearest canal or ravine.
While
the poorest of the poor get their water and get rid of their
waste in plastic bags, the rest are subject to the pay-as-you-go
free-market chaos of water and waste tanker-trucks, run almost
entirely by the local and international NGO private sector. A
sharp rise in petrol’s price, if some event, say, changes Hugo
Chavez's PetroCaribe deal under which Haiti gets cheap oil
largely on credit, could quickly deepen Haiti's water and
sanitation crisis.
DINEPA, Haiti’s National Water and Sanitation Agency founded in
2008, says around a dozen private companies collect and dispose
of sewage along with an unregistered number of manual merchant
toilet cleaners, know as “bayakou.” DINEPA could not
answer how many private water provision companies operate in
Haiti and directed the query to the Ministry of Commerce and
Industry, which sent the question back to DINEPA. There is
evidently no registration of water companies and no state
regulation of water quality.
Haiti is one of
the few countries in the world where water security has
deteriorated since the implementation in 2000 of the Millennium
Development Goals, while, since 2004, the UN has maintained a
multi-billion dollar military occupation in a country with no
war and one of the lowest homicide rates in the region.
Jon
Andrus, Deputy Director of the Pan American Health Organization
(PAHO), concedes that the privatization of Haiti’s water and
sanitation has threatened Haiti’s most vulnerable people and
that PAHO and partners "have failed for decades to reverse that
situation."
Andrus is
optimistic about the new plan having seen first hand the
eradication of polio, rubella, and measles in some of the
poorest parts of the world, despite “naysayers” even at high
levels of government.
The challenge of
raising $2.2 billion in the face of international donor fatigue
is not small, even though only 1% of post-earthquake funds
actually went to the Haitian government, and international
donors still owe Haiti $2.5 billion in unfulfilled pledges. The
U.S. alone has yet to come through on $650 million pledged in
post-earthquake “build back better” funds, which could neatly
cover the next two years of the cholera eradication plan.
“I
can’t think of another country where they built the
infrastructure from the ground up in an emergency context” said
Dr. Daniele Lantagne, a U.S. cholera expert specializing in
emergency water and sanitation interventions in developing
countries. Lantagne is one of the leading scientists who
concluded the UN’s camp of Nepalese soldiers in Mirebalais on
Haiti’s Central Plateau was “the most likely source of the
introduction of cholera into Haiti.”
On
Feb. 27, 2013, the UN billed the 10-year cholera eradication
plan as its own (the Haitian and Dominican governments had
originally proposed it in January 2012). Yann Libessart, the
communication officer of Doctors Without Borders (MSF), was not
impressed by the lofty rhetoric of UN Secretary General Ban Ki-moon
and others that day. Only $238 million, barely half of the
plan’s funding for the next two years, has been scraped
together, most of that ($215 million) coming from money already
pledged during the Mar. 31, 2010 post-earthquake UN conference.
Meanwhile cholera treatment centers which MSF passed on to the
government are currently “degenerating” into “contamination
zones,” he says. When asked who should fund the plan, Libessart
is blunt: “the people who are responsible for the introduction
of the disease into the country, for example.”
The
same sentiment was expressed by Dr. Ralph Ternier, Partners In
Health Director of Community Care and Support in the Central
Plateau, where cholera originated and persists today at a rate
double the national average.
“What’s important for this kind of institution is their image,”
said Ternier, not surprised by the UN’s parsimony on cholera
relief. “The fact that they’d give more money would mean they
are guilty.”
Emergency funds for cholera - only 2.5% of which ever went to
the Haitian government - dried up in January. Most NGOs have
left and the funding vacuum is squeezing DINEPA, putting the
water and sanitation jobs of two dozen qualified Haitians on the
firing line.
In
January, white UN sewage trucks could be seen offloading their
contents into the tailing ponds of Haiti’s first sewage
treatment plant in Morne à Cabrit. Now, that plant has been
closed for maintenance due to lack of operational funds. It
opened only 18 months ago.
Since
sewage treatment is central to stopping cholera, why aren’t
international funds forthcoming? “It beats me,” says Wilson
Etienne, a DINEPA official who oversaw the the building of the
treatment site.
DINEPA still aims to open two dozen treatment sites, one in each
urban center, but the only business model Etienne foresees
making this possible is one that charges $4 per cubic meter of
human waste.
For
now, the Morne à Cabrit plant remains closed. “This site should
have been something Haitians could be really proud of,” laments
Etienne, shaking his head.
An earlier version of this article was published in The Nation. |