|
Lack of financing for a ten-year
cholera eradication plan means that the disease will likely be
endemic to Haiti for years to come.
Cholera bacteria
are spread by contaminated food, water, and fecal matter. One of
the essential parts of the US$2.2 billion
National Plan for the
Elimination of Cholera in Haiti is the financing for sanitation
systems nationwide.
The majority of Haitians –
about eight million people – do not have access to a hygienic
sanitation system. They defecate in the open, in fields, in
ravines, and on riverbanks. The capital region produces over 900
tons of human excreta every day, according to the United Nations
Office for Project Services (UNOPS).
“Haiti is the only country in
the entire world whose sanitation coverage decreased in the last
decade,” said Dr. Rishi Rattan, a member of Physicians for
Haiti, an association of doctors and health professionals based
in Boston that works with Partners in Health and other Haitian
groups.
“Before the cholera outbreak or
the earthquake, diarrhea was the number one killer of children
under five and the second leading cause of all death in Haiti.
Given that cholera is a water-borne illness that relies upon
lack of access to clean water, it is highly likely that cholera
will become endemic in Haiti without full funding of Haiti's
cholera elimination plan by entities such as the United Nations
(UN),” Rattan told Haiti Grassroots Watch (HGW) in an email.
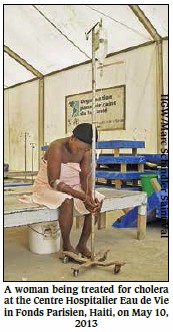
Cholera,
brought to Haiti in
October 2010 by soldiers from the United Nations Stabilization
Mission in Haiti (MINUSTAH), quickly spread throughout the
country. To date, over 600,000 people have been infected and at
least 8,160 have died, according to a government report dated
Jun. 30, 2013. Almost 3,000 people are infected each month.
The death rate is on the rise
in the countryside. Today, more than 4% of those infected die
due to the lack of cholera treatment centers. At the epidemic’s
peak, there were 285. Today, there are only 28. Once their
financing ran out, most humanitarian agencies abandoned the
country.
Worse, one of the two large
waste treatment facilities built following the earthquake
recently went out of service. [DINEPA just opened a third waste
treatment plant in Limonade on Jul. 24.]
The cholera-excrement connection
Written by the Pan-American Health
Organization (PAHO), the U.S. and Haitian governments, and
UNICEF, and published in November 2012, the cholera elimination
plan has as one of its main targets human excrement. The plan
sets as its objective that by 2022, “90% of the population has
access [to] and uses a functional sanitary facility” and that
“100% of drained excreta are treated before being discharged
into the natural environment.”
 The sanitation budget will cost
more than US$467 million.
“According to our figures, less
than 30% of the population has access to what we might call
basic sanitation,” according to Edwige Petit, head of sanitation
for the government’s National Agency of Water and Sanitation (in
French, Direction nationale de l’eau potable et de
l’assainissement - DINEPA). “In neighboring countries, 92%
to 98% have basic sanitation.”
By DINEPA’s count, about one
half of households in the countryside, and 10% to 20% in the
cities, does not have access to a proper toilet or latrine. They
must use rivers, ravines, or almost any open space to take care of
their needs.
In Cité Soleil, a slum that is
part of the metropolitan area, some people are forced to use any
open patch of ground they can find.
“As far as latrines are
concerned, we ‘go’ wherever we can, do you understand?”
explained resident Wisly Bellevue, without a blink. “In other
words, we go in the wild, nearby.”
“When our children have to take
a poop, we put them on a little bowl,” he said. “We put a little
water in there. Once they are done, we throw it into an empty
lot.”
Big institutions with septic
systems are serviced by excreta trucks managed by the state,
UNICEF, or other agencies, or by private companies. In 2010 and
2011, for example, humanitarian agencies emptied the thousands
of portable toilets (“Johnny-on-the-spot” or “Porta Potty”) in
the refugee camps for the 1.3 million people made homeless by
the 2010 earthquake.
Those who cannot pay for the
luxury provided by the trucks have to hire a more economical
service: the men called “bayakou” in Haiti, who empty
latrines and septic systems by hand.
The bayakou work at
night. Most of them do not take their excreta to the DINEPA’s
new waste treatment centers, and instead dump their cargos in
rivers, canals, and ravines. The workers sometimes even dump
their human output on the ground nearby if the rising sun
catches them at work, because, at all costs, they try to avoid
being identified by the population.
Before the cholera epidemic,
even the trucks used to dump their “black water” (feces mixed
with urine) into the ravines that drain into the Caribbean Sea.
Since the cholera outbreak, the government and other authorities
have been trying to convince all the sanitation actors to empty
their loads at locations that do not put people’s health in
danger.
In late 2010, DINEPA and UNICEF
opened a giant temporary site in Truitier, north of the capital,
to receive all of the material collected from the refugee camp
portable toilets as well as from other locations. At the time, a
DINEPA representative told HGW that the giant pool of excreta
was “the start of at least some form of excreta management” for
Haiti.
Advances and Challenges
Since then, DINEPA and its partners have
made considerable advances in sanitation. With assistance from
the Spanish government, UNICEF and others, DINEPA build two
treatment centers for the capital region’s black water, and
hopes to build 22 others for a total budget of US$159 million.
To date however, only one has been started.
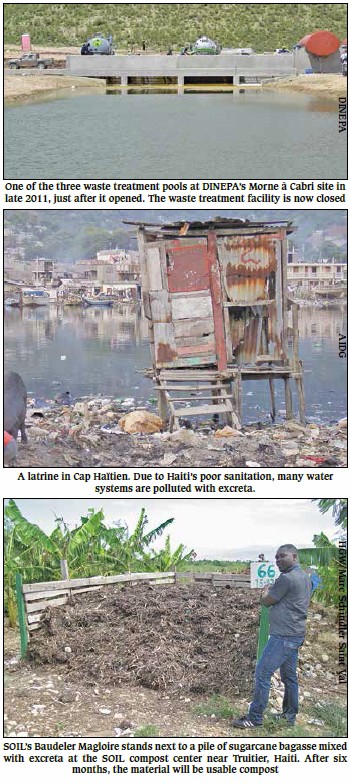
The impressive Morne à Cabri
waste treatment center, costing about US$2.5 million and
inaugurated in September 2011, “has the capacity to treat 500
cubic meters of excreta per day, which is the equivalent of what
500,000 produce,” according to DINEPA. But there is already a
problem.
Today, the center is closed
down. The excreta are not being delivered. The gates are locked.
Lack of financing is one reason. The fees paid by excreta
trucking companies don’t generate enough revenue.
Also, after the humanitarian
agencies stopped managing the refugee camps, because they said
they had no more financing, deliveries from the portable toilets
became problematic.
“We went from having latrine
matter being made up of 10% to 20% trash, to 70% to 80%,” Petit
explained. “The treatment center was not built to handle trash.
It was built to handle water and fecal matter. The pools
collapsed, blocked with trash.”
Even though it is struggling
financially, DINEPA is determined to get things working again.
“We are going to use government equipment. If we can get
US$40,000 or US$50,000 we will be able to clean it,” she said.
Of course, the other treatment
center is working, but one key challenge remains: how to
convince everyone to deliver his or her loads?
And even if the excreta are
delivered, financing will remain problematic. The excreta
trucking companies can pay, but the same is not guaranteed for
the bayakou. Perhaps this is why observers say the
journeymen continue to dump their loads wherever they can.
Frantz François is responsible
for sanitation and the gardens at a Cité Soleil community
center. “The bayakou do a bad job,” he said. “Right now,
at this moment, if you walk up and down the canal you will see
it is clean. But tomorrow, it will stink. They throw their
latrine loads wherever they want to.”
Another part of the national
cholera plan is national education campaigns aimed at combatting
“poor defecation and hygiene practices.” According to Petit,
many rural families don’t bother building latrines any longer;
they merely concentrate on building homes.
“Over the past 30 years, a
certain mentality has developed, where people know that it’s
quite possible somebody else [like a foreign agency] will give
them toilets,” Petit explained.
Rather than giving out free
toilets and latrines, DINEPA hopes to set up a US$120 million
fund that will allow families to borrow the money necessary to
do their own building.
An Alternative
DINEPA is not the only organization working
on the sanitation issue in Haiti. The U.S.-based
Sustainable
Organic Integrated Livelihoods (SOIL) treats and transforms
human excrement into compost that can be used as fertilizer.
SOIL supplies people and institutions who pay a small monthly
fee with special latrines. At least once a week, the
“Poopmobile” collects the excreta. So far, SOIL says there are
276 “Eco-san” toilets in operation around the country, serving
about 10,000 people.
SOIL’s compost installation is
located at Trutier, north of the capital, not far from one of
the two DINEPA waste treatment centers. Three people work there.
One empties the Poopmobile drums into the piles that become
usable compost after six months, while the others clean and
disinfect the drums so they can be reused.
“A lot of countries use this
system,” said Baudeler Magloire, project manager at SOIL. “Many
in West Africa. It is a new approach, a kind of ecological
sanitation.”
The approach is not completely
“new.” Human fecal matter has been used as fertilizer since the
ancient Chinese and Roman civilizations. The Aztec and Inca
peoples also used human excreta in their fields.
SOIL is not opposed to the
waste treatment “lakes” being used by DINEPA, but the objectives
are different, Magloire noted.
“Our mission is to allow for
the material to be recycled, transformed and then sent to places
in the country where it is needed,” he said. “People can buy it,
sell it, and use it in agriculture.”
Anti-cholera plan “in deep shit?”
While the Poopmobile collect fecal matter
from 24,000 latrines in a country of 10 million, three-quarters
of the population is still using non-hygienic practices and
systems.
The National Plan for the
Elimination of Cholera in Haiti requires US$2.2 billion, and a
plan for the neighboring Dominican Republic needs US$77 million
more. For the years 2013 and 2014 alone, the two countries are
seeking a total of US$521 million: US$443.7 for Haiti and US$33
for her neighbor.
The World Bank, PAHO, and
UNICEF recently promised US$29 million, and UN agencies have
offered another US$2.5 million. But, as of May 31 2013, the
pledges had not topped more than US$210 million, less than half
of what is needed.
“Investments in water and
sanitation are absolutely essential to eliminate cholera
transmission,” said PAHO Deputy Director Jon K. Andrus at a
Washington meeting where the grant was announced.
Andrus’ supervisor pleaded for
all donors to make commitments. “We must challenge governments
and partners to come up with the funds that are needed to get
the job done,” said PAHO Director Carissa F. Etienne. “The goal
is not just eliminating cholera. It is to ensure that every man,
woman, and child has access to safe water and sanitation. This
is basic to the dignity of every human being.”
Dr. Rattan of Physicians for
Haiti believes the UN should give the majority of the funding
needed, as soon as possible. “They have decreased the amount of
money they initially pledged and it has yet to actually be
disbursed,” Rattan wrote in a Jul. 17, 2013 email to HGW. “This
is crippling the Haitian government's ability to implement their
lifesaving cholera elimination plan.”
In Cité Soleil, Michelène
Milfort knows very well that there will be no plan implemented
any time soon. She lives in a tent with nine others. Her camp
has 38 deteriorating temporary shelters, tents, and shacks.
These earthquake victims only have three SOIL latrines to take
care of their needs. Before SOIL’s assistance, they used a
nearby empty lot.
John Abniel Poliné is a
neighbor. “Some people have no regular place to take care of
their needs,” he admitted. “Sometimes a person has to use a
little plastic bag, that he then throws into a canal. It is not
always the fault of the individual. You need to understand that
if the person had a place to go, he would not be forced to that
extreme.”
Poliné said he wonders about
the priorities of the Haitian government and of international
actors, especially MINUSTAH. “They just keep giving MINUSTAH
thousands of dollars, while the people of Cité Soleil live in
subhuman conditions,” he said.
MINUSTAH’s
2012-2013 budget is
US$638 million, over US$200 more than what is needed by the
Haiti and the Dominican Republic for the first two years of
their cholera elimination plans.
Haiti
Grassroots Watch
is a partnership of
AlterPresse,
the
Society of
the Animation of Social Communication (SAKS),
the Network of Women Community Radio Broadcasters (REFRAKA),
community radio stations from the Association of Haitian
Community Media and students from the Journalism Laboratory at
the State University of Haiti. |